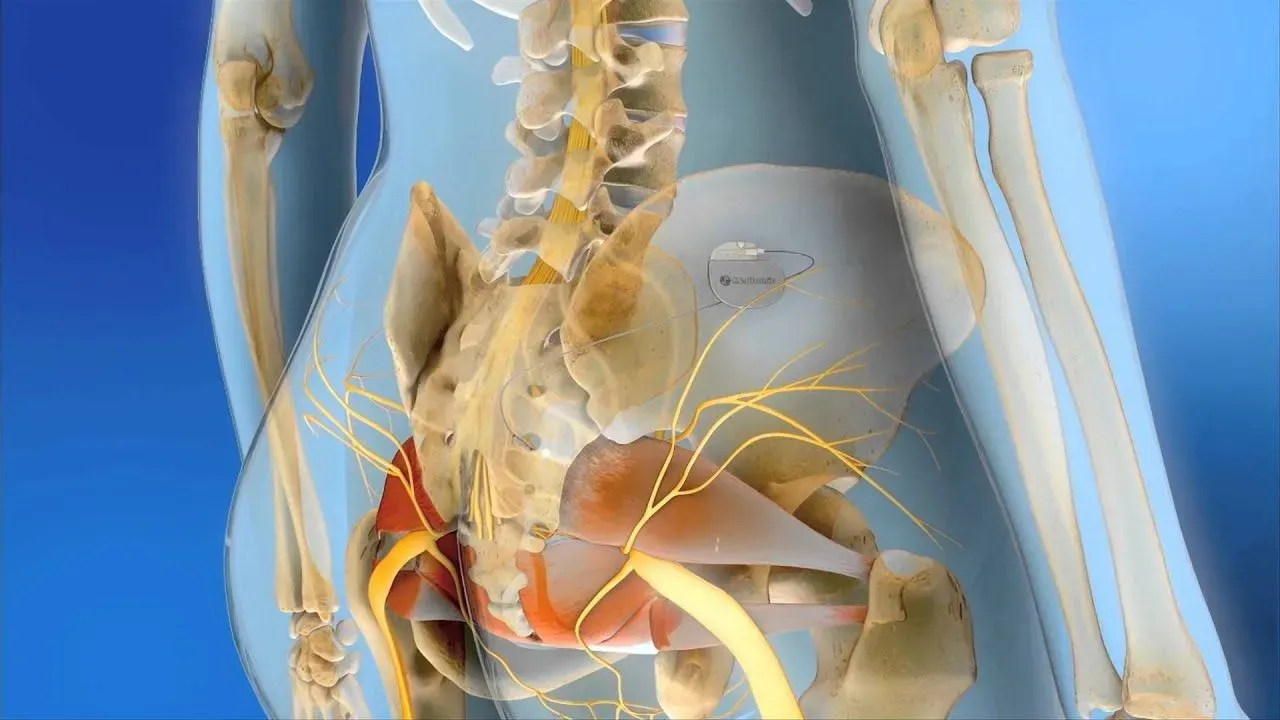
At our office in West Columbia sacral neuromodulation is a medical procedure that involves the placement of a small device, known as a neuromodulator, near the sacral nerves in the lower back. The sacral nerves are responsible for controlling the function of the bladder, bowel, and pelvic floor muscles.
The neuromodulator delivers mild electrical impulses to the sacral nerves to improve the communication between the nerves and the brain, helping to regulate the function of the bladder and bowel. This can effectively treat certain conditions such as overactive bladder, urinary retention, fecal incontinence, and chronic pelvic pain.
The procedure typically involves two stages. In the first stage, a temporary wire lead is inserted near the sacral nerves and connected to an external stimulator. This stage helps to determine if sacral neuromodulation is effective in relieving the symptoms. If the trial period is successful, in the second stage, a permanent stimulator device is implanted under the skin, usually in the upper buttock area, and connected to the lead.
Sacral neuromodulation is considered a reversible treatment option and can be adjusted or turned off if needed. It is generally recommended for individuals who have not responded well to other conservative treatments and have significant disruption in their quality of life due to bladder, bowel, or pelvic floor dysfunction.
If you have any questions, please contact us or make an appointment today. Call us at (803) 457-7000 or

Sacral neuromodulation is a long-term solution, but it is not considered a permanent solution for certain conditions. It is primarily used to manage symptoms of overactive bladder, urinary retention, and fecal incontinence that have not responded to other treatments. The effects of sacral neuromodulation can vary from person to person, and some individuals may require ongoing therapy or additional treatments in the future. It's important to discuss the expected outcomes and potential benefits and risks with a healthcare professional experienced in sacral neuromodulation to determine if it is the right option for you.
Sacral neuromodulation is generally considered to be a minimally invasive and relatively low-risk procedure. Most patients tolerate it well and report minimal pain or discomfort during and after the procedure. However, as with any medical intervention, individual experiences may vary. After sacral neuromodulation West Columbia patients may experience mild soreness or discomfort at the implant site, which is temporary and typically resolves within a few days. It is always best to consult with a healthcare professional who can provide personalized information and address any concerns specific to your case.
Sacral neuromodulation has shown to be an effective treatment option for certain bladder and bowel conditions. Studies have demonstrated its efficacy in managing symptoms of overactive bladder, urinary retention, and fecal incontinence that have not responded to other treatments.
For bladder conditions, such as overactive bladder, clinical trials have shown that sacral neuromodulation can significantly reduce urinary frequency, urgency, and incontinence episodes. Many patients experience improvement in their quality of life and an overall reduction in symptoms.
For certain bowel conditions, including fecal incontinence, sacral neuromodulation has also shown promising results. It can help improve control over bowel movements, reduce episodes of fecal incontinence, and improve overall bowel function.
However, it is important to note that the effectiveness of sacral neuromodulation may vary between individuals. It is best to consult with a healthcare professional experienced in this treatment to discuss your specific condition and determine if sacral neuromodulation is a suitable option for you.
The recovery period after sacral neuromodulation surgery can vary from person to person.
Like any surgical procedure, sacral neuromodulation carries some risks and potential complications. These risks can include:
Infection: There is a risk of infection at the surgical site, which may require further treatment, such as antibiotics or surgical intervention.
Pain or discomfort: Some individuals may experience temporary pain or discomfort at the implant site, which usually resolves within a few days or weeks.
Device-related issues: The implanted device may malfunction or require adjustments over time. This may include issues with the lead placement, battery life, or programming.
Allergic reaction: In rare cases, an allergic reaction to the materials used in the device or surgical procedures may occur.
Bleeding: There is a risk of bleeding during or after the surgery, which may require additional medical intervention.
Lead migration or dislodgment: The leads used in the procedure may move or become dislodged over time, potentially affecting the effectiveness of treatment.
In rare cases, nerve damage or bowel or bladder injury may occur during the surgery.

Southern Urogynecology has been designated an Axonics Center of Excellence by Axonics Modulation Technologies. The designation recognizes the Southern Urogynecology team and specifically the expertise of Dr. Andrea Pezzella for their expertise with Axonics Therapy, the quality of their patient outcomes, and their continued commitment to improving the lives of patients suffering from debilitating bladder and bowel symptoms.

Physicians included in the InterStim™ Center of Excellence (COE) program have been recognized by Medtronic for demonstrating exemplary use of the InterStim™ system and a commitment to patient care for those suffering from symptoms associated with overactive bladder (OAB), fecal incontinence (FI) and non-obstructive urinary retention.